What is Revenue Cycle Management?
Revenue Cycle Management (RCM) is a crucial process in healthcare that involves managing the financial aspects of patient care from start to finish. It includes patient registration, insurance verification, service documentation, billing, and collections. The goal is to ensure that healthcare providers receive timely and accurate payments for services rendered.
Efficient RCM improves cash flow, reduces claim denials, and enhances the overall financial health of a healthcare organization. By streamlining these processes, providers can focus more on patient care and less on administrative tasks.
Tips FOR Revenue Cycle Management
1. Stay Updated with Coding Changes
Keeping current with coding changes, such as updates to ICD-10 and CPT codes, is essential. This ensures that your claims are accurate and less likely to be denied, leading to faster reimbursements. Regular training and updates for coding staff can help maintain this accuracy.
2. Verify Patient Eligibility in Advance
Confirming a patient’s insurance coverage before their appointment can prevent claim denials. This proactive step helps to ensure that services are billable and covered, saving time and reducing billing errors.
3. Collect Payments Upfront
Implementing a policy to collect copays, deductibles, and coinsurance at the time of service improves cash flow. Train your staff to ask for these payments politely but firmly, ensuring patients understand their financial responsibilities.
4. Submit Clean Claims
Double-checking claims for errors before submission can significantly reduce denial rates. Using claims scrubbing software can automate this process, catching mistakes early and ensuring cleaner claims.
5. Promptly Address Denials
Act quickly to resolve denied claims by identifying the reasons and making necessary corrections. A dedicated team or process for handling denials can improve your recovery rate and reduce the backlog of unresolved claims.
6. Monitor and Benchmark Key Metrics
Track key performance indicators such as days in accounts receivable, clean claim rates, and denial rates. Regularly compare these metrics against industry benchmarks to identify areas needing improvement.
7. Embrace Advanced RCM Technology
Utilizing an integrated RCM platform can automate many processes, from eligibility checks to claims processing. This technology enhances efficiency, reduces errors, and provides comprehensive reporting.
8. Educate Patients on Financial Responsibilities
Clear communication about costs and insurance coverage helps patients understand their financial obligations. Providing this information upfront can lead to more timely payments and fewer billing disputes.
9. Streamline Patient Collections
Offering various payment options like online platforms, recurring payment plans, and automated reminders can make it easier for patients to pay their bills, improving your overall collections.
10. Collaborate with Payers
Building good relationships with insurance payers and understanding their policies can streamline the claims process. Participate in payer education sessions to stay informed about changes and best practices.
11. Implement a Proactive Denials Management Strategy
Establish a team focused on managing denials, identifying common causes, and implementing preventive measures. This proactive approach can reduce the occurrence of denials and improve overall claim success rates.
12. Conduct Regular Training for Staff
Ongoing education for billing and coding staff ensures they are up-to-date with the latest practices and regulations. Regular training can help maintain high standards and improve the accuracy of your claims.
What is revenue cycle management (RCM) in Healthcare?
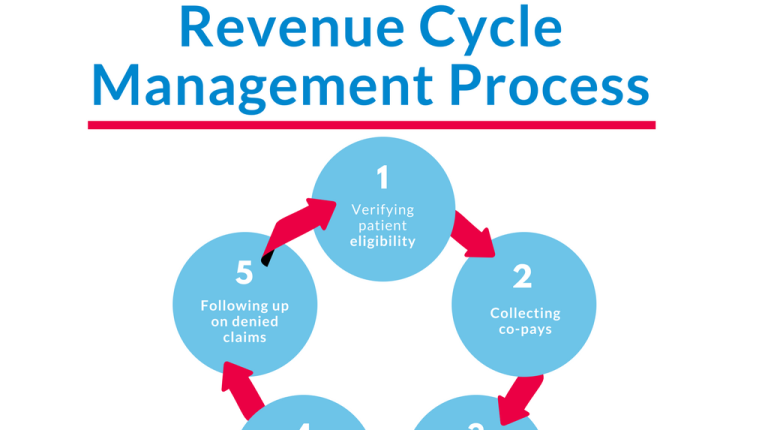
Revenue Cycle Management (RCM) in healthcare is the process of managing and optimizing the financial aspects of a medical practice or healthcare organization. It encompasses the entire journey of a patient’s financial experience from the initial appointment or service request through to the final payment of the bill. This includes several key stages:
- Patient Registration: Collecting and verifying patient information, including insurance details.
- Insurance Verification: Confirming coverage and benefits with the insurance provider.
- Coding and Documentation: Accurately coding medical diagnoses and procedures for billing purposes.
- Claim Submission: Sending claims to insurance companies for reimbursement.
- Follow-Up: Monitoring and managing claim status, addressing denials or rejections.
- Patient Billing: Issuing bills to patients for any remaining balance not covered by insurance.
- Payment Posting: Recording payments received from both insurance and patients.
- Account Reconciliation: Ensuring all transactions are accurately reflected in the practice’s financial records.
Effective RCM helps ensure that a healthcare provider receives appropriate reimbursement for services rendered while minimizing administrative errors and improving overall financial performance.